Understanding Aortic Aneurysms — What You Need to Know
An aortic aneurysm is a potentially life-threatening condition in which a section of the aorta — the body's largest artery — becomes abnormally enlarged. Because aortic aneurysms often develop silently without any noticeable symptoms, they are sometimes referred to as a "silent killer." Understanding this condition, knowing your risk factors, and being aware of screening and treatment options can genuinely save your life.
What Is an Aortic Aneurysm?
The aorta is the main artery that carries oxygen-rich blood from the heart to the rest of the body. It runs from the heart downward through the chest and abdomen before dividing into two branches that supply the legs. A healthy aorta is roughly the diameter of a garden hose, typically measuring around 2 centimetres across in the abdomen.
An aneurysm occurs when the wall of the aorta weakens and begins to bulge outward, much like a weak spot on an inflated tyre. As the aneurysm grows, the aortic wall becomes thinner and more fragile, increasing the risk of rupture. A ruptured aortic aneurysm is a surgical emergency with a very high mortality rate, which is why early detection and monitoring are so important.
Types of Aortic Aneurysms
Abdominal Aortic Aneurysm (AAA)
The most common type, abdominal aortic aneurysms occur in the section of the aorta that passes through the abdomen, typically below the kidneys. AAAs account for approximately 75% of all aortic aneurysms. They are most frequently found in men over the age of 65, particularly those with a history of smoking. Many AAAs are discovered incidentally during imaging studies performed for other reasons.
Thoracic Aortic Aneurysm (TAA)
Thoracic aortic aneurysms develop in the section of the aorta that runs through the chest. They are less common than AAAs but can be equally dangerous. TAAs may affect the ascending aorta (closest to the heart), the aortic arch, or the descending thoracic aorta. Some thoracic aneurysms are associated with connective tissue disorders such as Marfan syndrome or bicuspid aortic valve disease.
Thoracoabdominal Aneurysms
In some cases, an aneurysm extends from the chest down into the abdomen, involving both the thoracic and abdominal segments of the aorta. These are known as thoracoabdominal aneurysms and represent the most complex type to treat.
Risk Factors
Several factors increase the likelihood of developing an aortic aneurysm:
- Smoking — this is the single most significant modifiable risk factor; smoking damages the aortic wall and accelerates aneurysm growth
- Age — the risk increases significantly after age 60, with most aneurysms diagnosed in patients aged 65 to 75
- Male sex — men are four to six times more likely to develop an AAA than women
- Family history — having a first-degree relative (parent or sibling) with an aortic aneurysm significantly increases your risk
- High blood pressure — chronic hypertension places ongoing stress on the aortic wall, contributing to its weakening
- Atherosclerosis — the build-up of fatty deposits in the artery walls can weaken the aorta over time
- Connective tissue disorders — conditions such as Marfan syndrome, Ehlers-Danlos syndrome, and Loeys-Dietz syndrome affect the structural integrity of blood vessel walls
Screening Recommendations
Because most aortic aneurysms are asymptomatic until they rupture, screening plays a vital role in early detection. Current guidelines recommend the following:
- Men aged 65 to 75 who have ever smoked should have a one-time ultrasound screening for AAA
- Men and women with a family history of AAA should discuss screening with their doctor, ideally starting at age 55 to 60
- Patients with connective tissue disorders should undergo regular imaging surveillance of the entire aorta
Screening is quick, painless, and non-invasive. An abdominal ultrasound can reliably measure the diameter of the aorta and detect aneurysms that require monitoring or intervention.
Treatment Options
The treatment approach for an aortic aneurysm depends on its size, rate of growth, location, and the patient's overall health. The three main strategies are:
Surveillance (Watchful Waiting)
Small aneurysms that have not yet reached the threshold for repair are monitored with regular ultrasound or CT scans. For abdominal aortic aneurysms, this typically means those measuring less than 5.5 cm in men or 5.0 cm in women. During surveillance, efforts focus on reducing risk factors: stopping smoking, controlling blood pressure, and managing cholesterol. Patients are usually scanned every 6 to 12 months to track any changes in size.
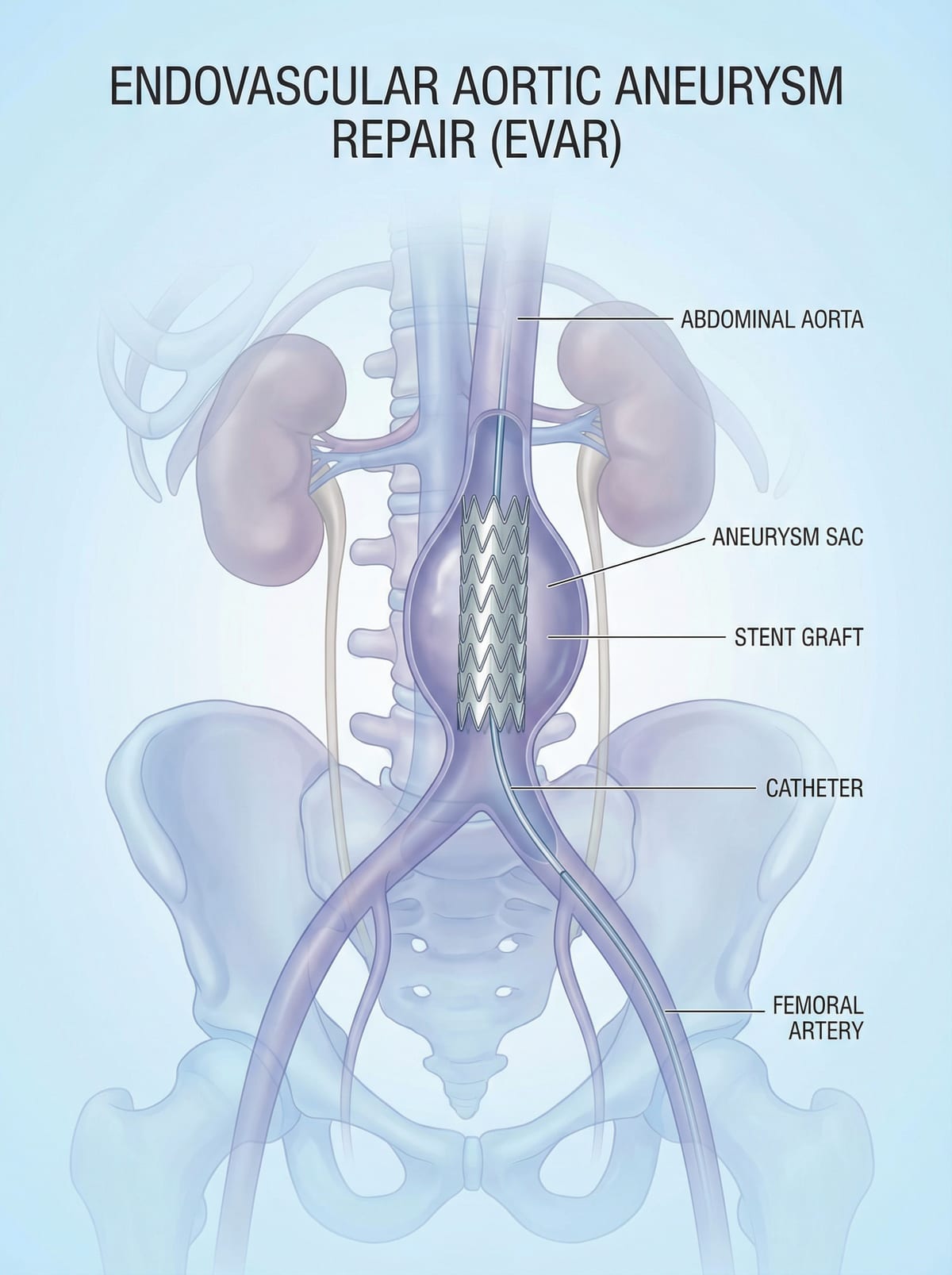
Endovascular Aneurysm Repair (EVAR)
EVAR is a minimally invasive procedure that has revolutionised the treatment of aortic aneurysms. Through small incisions in the groin, a synthetic graft (stent-graft) is guided through the femoral arteries under X-ray imaging and positioned inside the aneurysm. The stent-graft lines the weakened section of the aorta, redirecting blood flow through the graft and taking pressure off the aneurysm wall. EVAR offers significant advantages, including shorter hospital stays (typically 1 to 3 days), less pain, and faster recovery compared to open surgery. Most patients return to normal activities within 2 to 4 weeks.
Open Surgical Repair
Open repair involves a larger incision in the abdomen or chest to directly access the aorta. The diseased section is replaced with a synthetic graft sewn into place. While open surgery is more invasive and requires a longer recovery period (typically 5 to 10 days in hospital and several weeks of convalescence), it remains an important option for certain aneurysm configurations that are not suitable for endovascular repair. Open repair has been performed successfully for decades and provides excellent long-term durability.
Emergency Signs — When to Call for Help Immediately
A ruptured or rapidly expanding aortic aneurysm is a medical emergency. Call emergency services immediately if you or someone you know experiences:
- Sudden, severe abdominal or back pain — often described as a tearing or ripping sensation that comes on without warning
- Pain radiating to the back, flank, or groin — the pain may shift as blood leaks from the aneurysm
- Dizziness, lightheadedness, or fainting — signs of internal bleeding and dropping blood pressure
- Rapid pulse with clammy skin — your body's response to significant blood loss
- Sudden onset of nausea and vomiting with abdominal pain — which may mimic other abdominal emergencies
Time is critical in these situations. Survival rates for ruptured aneurysms are dramatically higher when patients reach a vascular surgeon quickly. This is why screening and elective repair of large aneurysms before they rupture is so important.
Living with an Aortic Aneurysm
If you have been diagnosed with a small aortic aneurysm that does not yet require repair, the most important steps you can take are to stop smoking (if applicable), keep your blood pressure well controlled, attend all scheduled surveillance appointments, and report any new symptoms to your doctor promptly. With careful monitoring and timely intervention when needed, patients with aortic aneurysms can lead full, active lives.
Dr. Medani has extensive experience in both endovascular and open surgical management of aortic aneurysms. If you have been diagnosed with an aneurysm, have risk factors that warrant screening, or simply want to discuss your vascular health, do not hesitate to arrange a consultation.