What is Thoracic Outlet Syndrome?
Thoracic outlet syndrome (TOS) is a group of conditions that occur when the blood vessels or nerves in the thoracic outlet — the space between the collarbone and the first rib — become compressed. This relatively uncommon but often misdiagnosed condition can cause pain, numbness, and weakness in the shoulder, arm, and hand. For patients who have been searching for answers to persistent arm symptoms, understanding TOS can be the first step toward effective treatment and relief.
Understanding the Thoracic Outlet
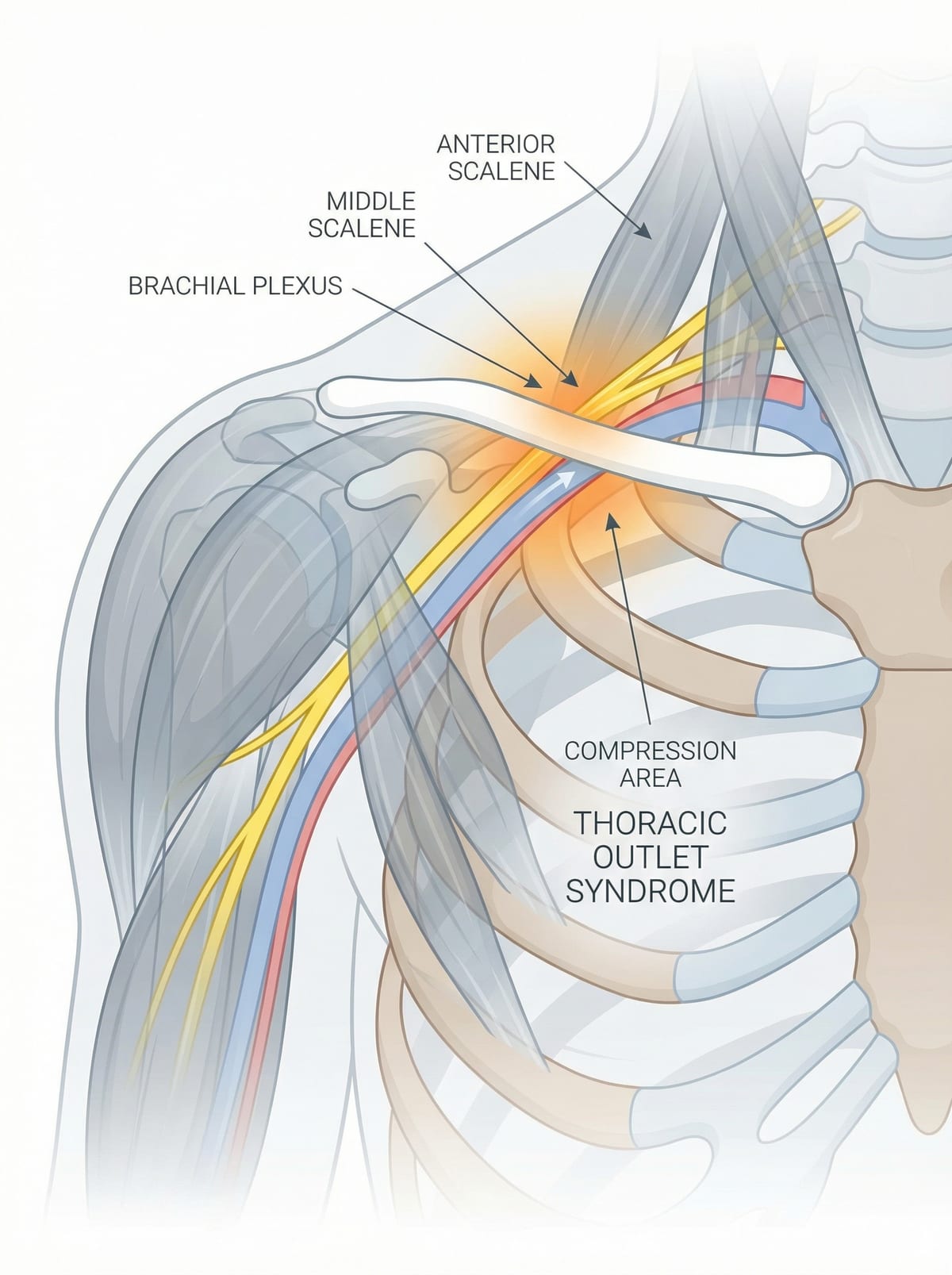
The thoracic outlet is a narrow passageway located at the base of the neck, just behind the collarbone. Through this small space pass several critical structures: the brachial plexus (the network of nerves that controls movement and sensation in the arm and hand), the subclavian artery (which supplies blood to the arm), and the subclavian vein (which drains blood from the arm back toward the heart).
The boundaries of the thoracic outlet are formed by the scalene muscles at the front, the first rib below, and the collarbone above. Any factor that narrows this already tight space — whether an extra rib, muscle enlargement, scarring from trauma, or repetitive overhead activities — can compress the nerves or blood vessels passing through it and produce symptoms.
Types of Thoracic Outlet Syndrome
TOS is classified into three types based on which structures are compressed. The type determines the symptoms and guides the treatment approach.
Neurogenic TOS (nTOS)
Neurogenic TOS is by far the most common form, accounting for approximately 95% of all TOS cases. It occurs when the nerves of the brachial plexus are compressed. Patients typically experience pain, numbness, tingling, and weakness in the arm and hand. Symptoms are often aggravated by overhead activities such as reaching, lifting, or even blow-drying hair. The small muscles at the base of the thumb may waste over time (thenar atrophy), and patients may notice difficulty with fine motor tasks such as buttoning a shirt or gripping objects.
Venous TOS (vTOS)
Venous TOS occurs when the subclavian vein is compressed, restricting the drainage of blood from the arm. This type accounts for roughly 3 to 5% of TOS cases. The hallmark presentation is sudden swelling of the entire arm, which may appear bluish or discoloured. The arm may feel heavy and aching. In some cases, a blood clot (deep vein thrombosis) forms in the subclavian vein — a condition sometimes called Paget-Schroetter syndrome or "effort thrombosis" because it often occurs in young, physically active individuals after vigorous upper-body activity.
Arterial TOS (aTOS)
Arterial TOS is the rarest and most serious form, accounting for approximately 1% of cases. It results from compression of the subclavian artery, typically by a cervical rib (an extra rib present from birth) or a bony abnormality of the first rib. Arterial compression can lead to damage of the artery wall, formation of blood clots, and in severe cases, embolisation (clots travelling to the hand and fingers), which can threaten the viability of the fingers. Symptoms include coldness, pallor, and pain in the hand, and sometimes small painful spots on the fingertips from emboli.
Symptoms to Watch For
The symptoms of TOS vary depending on the type but may include any combination of the following:
- Pain in the neck, shoulder, arm, or hand — often worsened by overhead activities or carrying heavy objects
- Numbness and tingling in the fingers, particularly the ring and little fingers
- Weakness in the hand and difficulty gripping
- Swelling and discolouration of the arm (in venous TOS)
- Coldness and colour changes in the hand and fingers (in arterial TOS)
- A feeling of heaviness or fatigue in the arm with use
- Symptoms that worsen when raising the arms overhead or when carrying bags
The Challenge of Diagnosis
Thoracic outlet syndrome, particularly the neurogenic type, is one of the most frequently misdiagnosed conditions in vascular and musculoskeletal medicine. The symptoms overlap significantly with other conditions, including cervical disc disease, carpal tunnel syndrome, rotator cuff problems, and even fibromyalgia. Many patients see multiple specialists and undergo numerous investigations over months or even years before receiving an accurate diagnosis.
There is no single definitive test for neurogenic TOS. Diagnosis relies on a thorough clinical evaluation, including a detailed history of the symptoms, physical examination with specific provocative manoeuvres (such as the elevated arm stress test and Adson's test), and a combination of investigations that may include:
- Chest X-ray — to identify a cervical rib or elongated transverse process of the C7 vertebra
- Duplex ultrasound — to assess blood flow in the subclavian artery and vein, often performed with the arm in different positions
- CT angiography or MR angiography — to visualise vascular compression and identify any anatomical variants
- Nerve conduction studies — which may be normal in many cases of nTOS, making the diagnosis more challenging
- Scalene muscle block — a diagnostic injection of local anaesthetic into the anterior scalene muscle; temporary relief of symptoms supports the diagnosis of nTOS
Treatment Options
Treatment for thoracic outlet syndrome depends on the type and severity of the condition. A stepwise approach is typically recommended, starting with conservative measures and progressing to surgical intervention when necessary.
Physiotherapy and Conservative Management
For neurogenic TOS, the first line of treatment is a structured physiotherapy programme lasting a minimum of 3 to 6 months. The goals of physiotherapy include stretching the scalene and pectoralis minor muscles to open up the thoracic outlet, strengthening the muscles that support proper posture and shoulder mechanics, correcting postural imbalances (particularly forward head posture and rounded shoulders), and learning activity modification to avoid aggravating positions. Many patients experience significant improvement with dedicated physiotherapy, particularly when combined with ergonomic adjustments at work and home.
Surgical Decompression
Surgery is considered when conservative treatment has failed to provide adequate relief after a reasonable trial period, or when the condition involves vascular compression (venous or arterial TOS), which typically requires more urgent intervention. The primary surgical procedure for TOS is first rib resection with scalenectomy. This operation involves removing the first rib and releasing the scalene muscles to create more space in the thoracic outlet and decompress the affected nerves or blood vessels.
The surgery can be performed through several approaches, including transaxillary (through the armpit), supraclavicular (above the collarbone), or a combination of both, depending on the specific anatomy and the structures involved. For venous TOS with thrombosis, treatment often begins with catheter-directed thrombolysis (clot-dissolving medication) followed by surgical decompression. For arterial TOS, surgery typically includes first rib resection along with reconstruction of the damaged artery.
Dr. Medani's Expertise in Thoracic Outlet Syndrome
Thoracic outlet syndrome is an area of particular interest and expertise for Dr. Medani. Having trained in major UK vascular centres where TOS is managed in dedicated multidisciplinary clinics, Dr. Medani brings extensive experience in the diagnosis and treatment of all three types of TOS. He understands the frustration that many TOS patients experience after years of unexplained symptoms and misdiagnosis, and he takes a thorough, patient-centred approach to evaluation.
Dr. Medani works closely with specialist physiotherapists to optimise conservative management and carefully selects patients for surgery based on clear clinical criteria. For those who do require surgical decompression, he performs first rib resection using meticulous technique to ensure safe and effective relief of compression while minimising the risk of complications.
If you have been experiencing persistent arm pain, numbness, swelling, or weakness that has not been explained by other diagnoses, thoracic outlet syndrome may be worth considering. A thorough vascular assessment can help determine whether TOS is the cause of your symptoms and guide you toward the right treatment pathway.